The Importance of End-to-End Encryption and Integrated Products
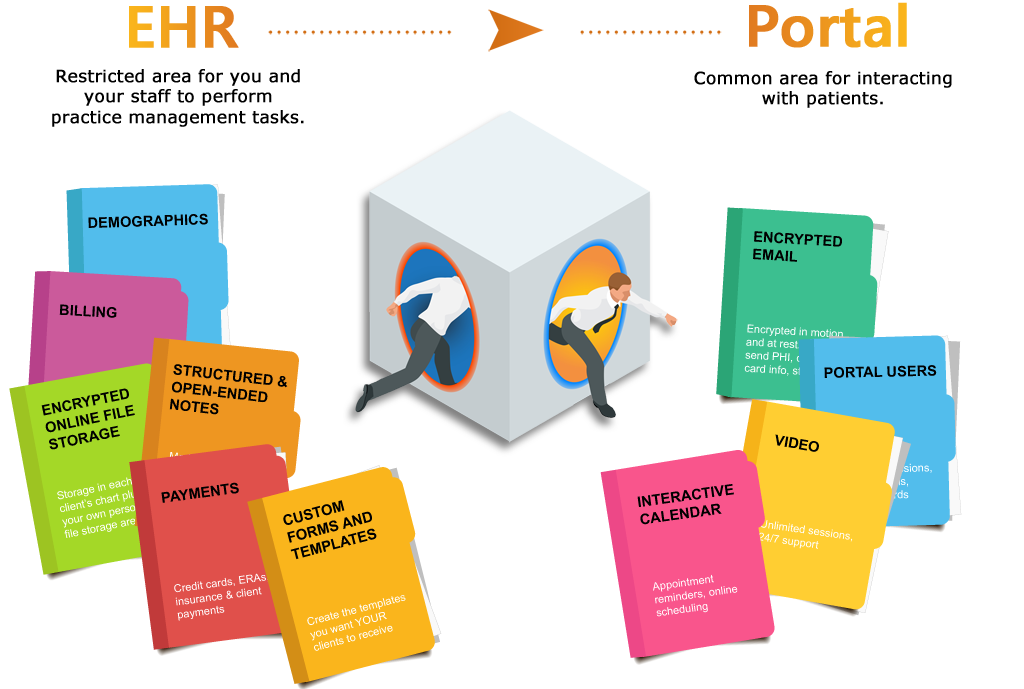
HIPAA is a frightening thing to many behavioral health providers. Although it is something to take seriously, it need not be frightening . Nor do you need to pay big bucks to a company to set things up for you. A very simple thing that will help you become compliant is to get an EHR that is both integrated and features end-to-end encryption. This post explains why.